Blog
Art and Science II: The Great Psychotherapy Debate
For the better part of a year, I have been reading Bruce Wampold’s book, The Great Psychotherapy Debate. It’s a white paper examining the evidence for two competing models of interpreting the research on outcomes in psychotherapy. The competing models for interpreting the research are The Medical Model and The Contextual Model...
I
For the better part of a year I have been reading Bruce Wampold’s book, The Great Psychotherapy Debate. It’s a white paper examining the evidence for two competing models of interpreting the research on outcomes in psychotherapy. The competing models for interpreting the research are The Medical Model and The Contextual Model.
The Medical Model posits that mental illnesses are like any other disease. In medicine, to treat a disease, we develop treatments with specific ingredients that remedy the particular deficits that cause the symptoms.
The Contextual Model posits that treatments with a cogent rationale accepted by the client, administered by a clinician who the client has a therapeutic relationship with, and involving therapeutic actions that the client expects will help, will lead to a health-promoting change.
The book frames this examination by using the ideas of one of my favorite philosophers of science, Imre Lakatos. It outlines how these two models act as competing research programmes. To get an idea of what that means, you can listen to Lakatos describe his theory on the philosophy of science in this lecture he gave to the BBC:
Philosophers of science argue about what should be considered science vs what should be considered pseudoscience. This is called “the demarcation problem.” Karl Popper believed the most important part of the demarcation problem was that a theory must be falsifiable to be called science (for a great critique of Popper’s position see fakenous’ article). Thomas Kuhn described science in a more sociological way, where “normal science” is disrupted by anomalies which led to the paradigm shift of a scientific revolution.
Lakatos’ view on science is to call something a scientific research programme if it has theories that explain observations and has had novel predictions that could have been falsified. Various research programmes exist at the same time, each with a hard core of theories that cannot be abandoned without abandoning the programme altogether. This hard core is protected by more modest and specific auxiliary hypotheses which help interpret data which seems anomalous. These auxiliary hypotheses can be generated or abandoned as needed. A research programme is progressive if it’s changes to its auxiliary hypotheses help it explain and predict new data and degenerative if it has been doing a poor job at explaining/predicting new data.
This view was an attempt to blend the normative views of Popper with the revolutionary structure described by Kuhn. But Lakatos thought Kuhn’s version of “normal science” and “revolution” were oversimplified, instead describing research programmes gaining adherents if they were more progressive rather than spurring a radical paradigm shift. His demarcation involves calling ‘science’ that which has a history of novel predictions (a programme) and which is progressive (updating in a successful way) in its ongoing explanations of and predictions for incoming data.
II
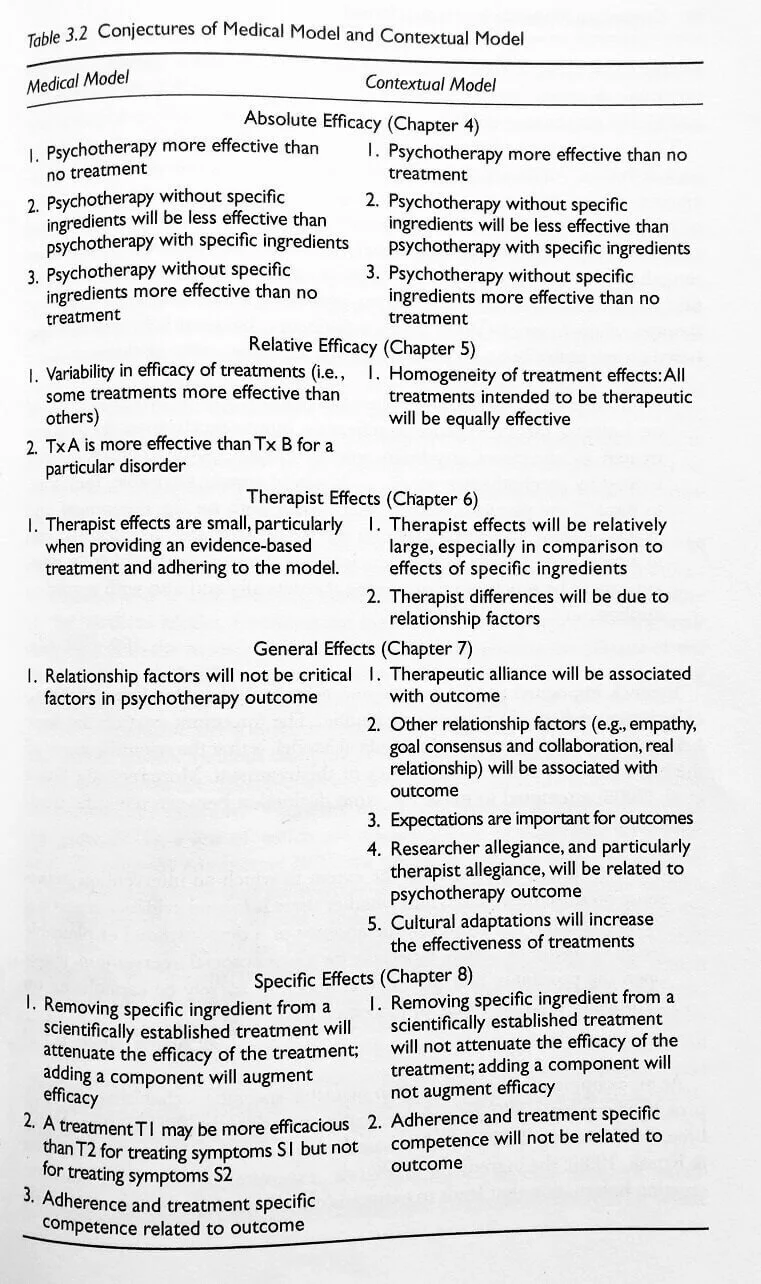
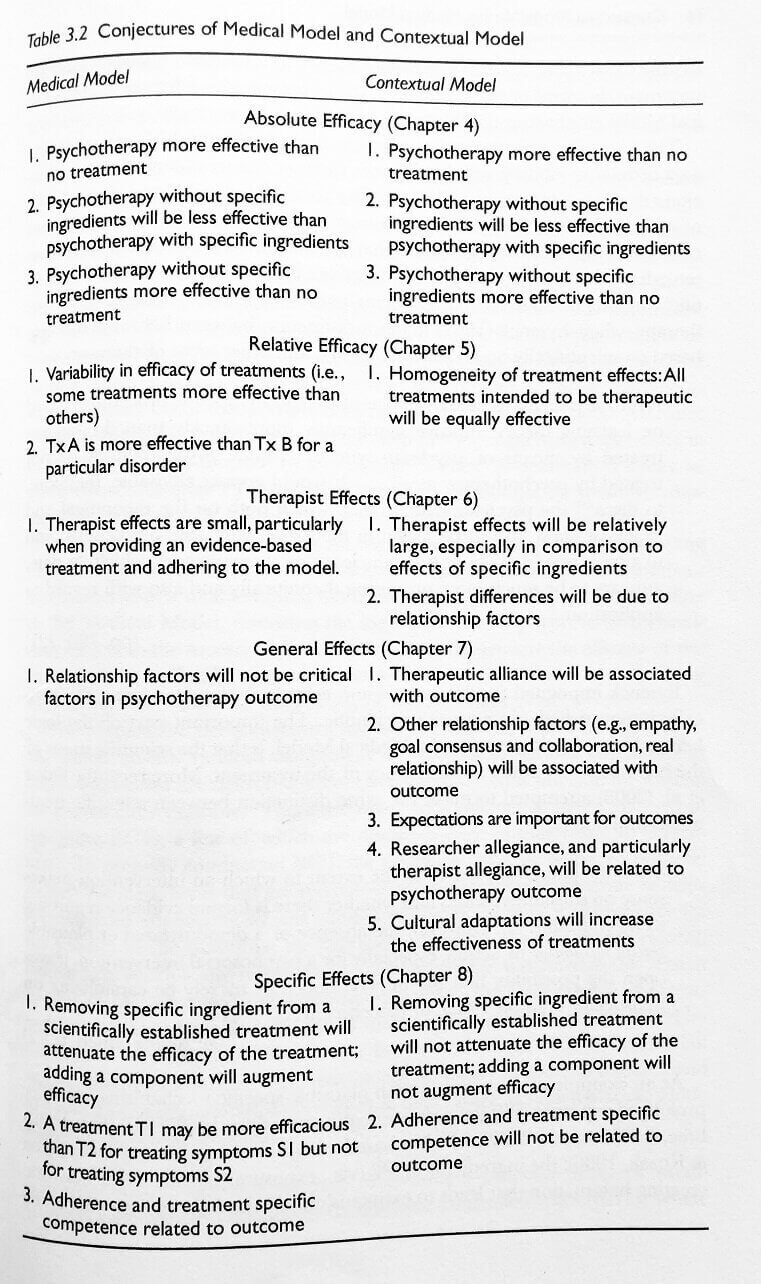
The Medical Model and The Contextual Model are two different research programmes which make very close predictions. But there are specific ways the hypotheses can be teased apart and tested and I think The Contextual Model is the more progressive programme. Here is the table from The Great Psychotherapy Debate where Wampold lays out the conjectures of each programme:
These are a list of conjectures that each research programme makes in order to predict and interpret data on the practice of psychotherapy and the results of psychotherapy outcomes research. Notice the predictions for "absolute efficacy" are identical in both models. The models diverge from there in examinations of "relative efficacy," "therapist effects," "general effects," and "specific effects."
Last year I spoke to one of my professors who was the director of the MFT program at CSULB which I attended. She's a trauma researcher and allied to The Medical Model. In our conversation about what works in treatment, I was arguing for The Contextual Model, saying I believed "relationship factors" are more important than "specific ingredients." (Contextual Model 6.1-6.2)
She argued that treatment for post traumatic stress disorder (PTSD) proved that The Medical Model was correct, saying , "I've had many patients come into treatment with me who had a great relationship with their previous therapist but their PTSD symptoms had not gone away. But upon doing prolonged exposure treatment in my clinic, their symptoms went away." Her claim was that a specific ingredient (prolonged exposure) is necessary for the effective treatment of PTSD. (Medical Model 8.1)
Both models predict that some sort of specific ingredient is necessary (Medical Model 4.2, Contextual Model 4.2). So what is the difference between what they’re claiming?
The Medical Model claims that specific ingredients target specific symptoms and therefore, adherence to a specific manual for treatment will be associated with outcome (Medical Model 8.1, 8.3). The Contextual Model claims you need a number of things to get a positive outcome: 1. A relationship 2. An adaptive rationale for the problem which is accepted by patient and therapist which provides hope and expectancy for change 3. A ritual which the patient and therapist perform into which effort is exerted. It’s claim is therefore that you need a clear explanation and ritual but the removal of a particular specific ingredient will not be associated with outcome. (Contextual Model 8.1-8.2)
That is to say - Dr Ghafoori was right to say that the strong relationship is not enough. Both models predict that a relationship without a clearly defined rationale for treatment and a ritual to be performed for treatment will be insufficient.
But her interpretation of The Medical Model would predict that any treatment lacking in exposure would not alleviate PTSD symptoms. The hypothesis she implied is directly out of The Medical Model: competence with and adherence to a treatment manual involving exposure will predict outcomes (Medical Model 8.3). Alternatively, The Contextual Model’s hypothesis is that a ritual that is accepted by the client and therapist must be performed (Contextual Model 4.2) but it will be therapeutic alliance, relationship factors, expectations, allegiance to the treatment, and culturally appropriate adaptations which predict outcomes (Contextual Model 7.1, 7.2, 7.3, 7.4, 7.5).
III
How can we test this? Well, first we can look at what The Medical Model says about PTSD. The medical model predicts there are specific ingredients that are required for successful symptom reduction: 1. targeting triggering stimulus through exposure to extinguish the affective response 2. targeting negative thoughts and beliefs that arise after the traumatic event through cognitive restructuring.
A treatment for PTSD was developed with neither of these specific ingredients. This treatment was called Present Centered Therapy and was developed initially as a pseudo-placebo control that had a cogent rationale (adaptive explanation) and therapeutic actions (a ritual). A 2014 meta analysis determined this treatments effectiveness was similar to previously established Evidence Based Treatments for PTSD such as Prolonged Exposure.
The effectiveness of a treatment without the specific ingredients hypothesized as necessary by The Medical Model directly contradicts it's prediction (Medical Model 8.2, 8.3)
So now we have to ask if the predictions of The Contextual Model (Contextual Model 7.1, 7.2, 7.3, 7.4, 7.5) do a better job.
Is therapeutic alliance associated with outcome? (Contextual Model 7.1)
Yes: “In sum, the overall relation between alliance and outcome in individual psychotherapy is robust, not effected by the file drawer problem, and accounts for approximately 7.5% of the variance in treatment outcomes.” (Horvath et al. 2011)
Are relationship factors associated with outcome? (Contextual Model 7.2)
Yes: The APA’s task force on Evidence-Based Relationships and Responsiveness considers collaborative relationships including goal consensus, empathy, feedback, and a positive regard as a demonstrably effective in enhancing psychotherapy outcomes. (APA 2019)
Are expectations important for outcomes? (Contextual Model 7.3)
Everyone seems to cite neuroscientist Fabrizio Benedetti on this. The most relevant quote I could find from him seems to suggest that yes, they are important: “Hidden administration of therapies has provided compelling evidence that expectation is a key element in therapeutic outcome (Benedetti et al., 2011c, Colloca et al., 2004). If the patient is unaware that a treatment is being performed and has no expectations about any clinical improvement, the therapy is not as efficacious. This has profound implications in terms of medical practice because the information delivered by health professionals can impact therapeutic outcome.” (Benedetti 2013)
Is researcher allegiance related to psychotherapy outcomes? (Contextual Model 7.4)
Yes: “Researcher allegiance (RA)-outcome association was robust across several moderating variables including characteristics of treatment, population, and the type of RA assessment. Allegiance towards the RA bias hypothesis moderated the RA-outcome association. The findings of this meta-meta-analysis suggest that the RA-outcome association is substantial and robust.” (Munder et al. 2013)
Are culturally adapted treatments more effective? (Contextual Model 7.5)
Yes: “The results provide evidence that culturally adapted psychotherapy produces superior outcomes for ethnic and racial minority clients over conventional psychotherapy by d = 0.32. The outcome differences favoring culturally adapted treatment were moderated solely by cultural adaptations of illness myth” (Benish et al. 2011)
IV
The Medical Model and The Contextual Model are competing research programmes. Presently, The Medical Model is the dominant research programme or, in Kuhn’s terms, the “normal science” of our field. The researchers within The Medical Model have been developing Evidence Based Treatments (EBTs) that contain specific ingredients to target specific symptoms for decades. But our outcomes are stagnant. Despite the efforts to develop EBTs, psychotherapy hasn’t improved in its ability to help people since we began measuring its effectiveness in helping people in the 70s. Since the project to develop specific treatments to remediate the symptoms of psychological disorders hasn’t borne out the promise of better outcomes in treatment, The Medical Model is a degenerative research programme.
The Contextual Model makes a number of predictions about what accounts for outcomes in psychotherapy. There’s an enormous amount of variation in the quality of scientific evidence but I believe the meta analyses and expert reviews I’ve linked here are high quality. The predictions of the contextual model have been borne out in the data. Taking the Lakatosian view, I believe the accuracy in the explanations and predictions of The Contextual Model make it the more progressive research programme. The Contextual Model is still a minority voice but I predict that over the next 10 years, The Contextual Model will gain adherents more rapidly than The Medical Model.
The Great Psychotherapy Debate has taken me about a year to get through. I haven’t been able to digest all the parts of The Contextual Model. I feel uneasy in regards to what it suggests about the role that specific ingredients play in psychotherapy. But perhaps my concerns there are tangent to what The Contextual Model actually says. The aim of The Contextual Model is to change our focus so that we can more reliably improve outcomes in psychotherapy. I’m on this ride so let’s see where this paradigm shift takes us.
Art and Science I: Please hold the Science
When I bring up the research from clinical psychology on outcomes of psychotherapy, other therapists say to me, “Psychotherapy is an art and a science.” Yet I’ve had one colleague say to me, “Science can’t tell us anything since it’s always changing its mind.” Another told me, “Science cannot reveal anything about therapy because therapy is about human relationships...”
I was at a cafeteria and ordered psychotherapy without science. The waiter said, “Sorry, we’re all out of science. Is psychotherapy without art okay?”
I
When I bring up the research from clinical psychology on outcomes of psychotherapy other therapists say to me, “psychotherapy is an art and a science.” Yet I’ve had one colleague say to me, “science can’t tell us anything since it’s always changing it’s mind.” Another told me, “science cannot reveal anything about therapy because therapy is about human relationships.” These are statements of “psychotherapy without science.”
I try to spend time getting to know the scientific, empirical, naturalistic paradigm as I believe it is the best tool to predict what will happen and is thus essential for determining how to act. Fortunately, there are groups of clinicians who are interested in the difficult exploration of researching the outcomes of psychotherapy and how it might help us understand how to actually be helpful rather than just intending to be helpful.
II
In the 50s, Hans Eysenck took a hard shot across the bow of our field by publishing a paper examining the evidence of whether psychotherapy helped a group of people with (what were called at the time) neurotic disorders. He looked at the evidence he collected and concluded that psychotherapy didn’t work! This led to a wave of responses and the application of Meta Analysis to studies on psychotherapy in a seminal work by Smith and Glass, “Meta-Analysis of Psychotherapy Outcome Studies.” Their expansive study contradicted Eysenck, concluding that psychotherapy had a demonstrable and significant positive effect with about 75% of people who were treated better off than those who did not receive treatment.
Today, the American Psychological Association has a statement with references to the extensive evidence covering decades of research which recognizes the well established effectiveness of psychotherapy. I have to explain a little about how they determine this. Psychotherapy’s effectiveness in helping people is assessed in a number of ways: self report, other report, clinician assessment, or metrics such as number of hospital visits or number of suicide attempts. It is measured in “effect size,” a measure of the distance between the means of two groups measured in standard deviations. In almost any way we assess psychotherapy, the effect size comes out at around 0.8, which is considered a large effect size and corresponds to 79% of the treated being better off than the untreated. This means the outcome of psychotherapy is similar to well established medical interventions such as coronary bypass surgery, arthritis medication, and AZT for AIDS.
Psychotherapy works.
III
After graduating with my master’s degree I found myself working in a group practice in New York. A friend from my clinical supervision group turned me on to a podcast about common factors theory. In the podcast, they suggested there was good evidence that the specific things said in therapy were not what determined outcomes but rather there was something else that was common to many different styles of psychotherapy that seems to determine outcomes. This led me to the authoritative book on the matter, The Heart and Soul of Change: Delivering What Works In Therapy. The evidence was solid and my confidence was shaken… I spent so much time in graduate school learning what to say and what not to say and those ‘specific ingredients’ didn’t seem to matter! I felt as though I had been misled… as though I was misguided in my work as a clinician. My clients noticed the change in me and half of them dropped me as their therapist.
I found myself at a loss. We have many pretenses about what it means to say that science supports psychotherapy… or that psychotherapy is scientific. But the research on outcomes seems to show that the specific ingredients in what we say aren’t what makes the difference. So why do we spend so much time and effort on “Evidence Based Treatments” that teach you what to say?
IV
I’ve long felt reluctant to discuss what actually seems to account for the outcomes in psychotherapy. There’s this threat that revealing it might take its power away. If we peek behind the curtain to see the wizard, does he lose his power? Part of this is due to the initial conclusion I drew from reading The Heart and Soul of Change: if there isn’t a difference in outcomes between the wildly divergent styles of psychotherapy, could it be that it’s merely a placebo?
The different styles of psychotherapy all contain essential common factors that help people change. This is one of the areas of research that Bruce Wampold focuses on. In a recent paper he discusses his finding that common factors predicts outcomes better than the specific ingredients that evidence based treatments focus on. Because of this, Wampold proposes we think about psychotherapy through a contextual model (which focuses on the healing relationship) rather than a medical model (which focuses on providing the treatment which heals). His research shows that the better we deliver the parts of the contextual model, the better the outcomes.
This is where I get perplexed. Is this how a placebo works? Does that word fit at all at this point or is it a concept out of place?
V
A few weeks ago I got to spend some time with Scott Alexander of SlateStarCodex. While talking to him about what makes psychotherapy work, I came upon another way to think about it. Maybe different styles of psychotherapy are all good enough approximations for our underlying psychology, are not fundamentally different, and thus something like a transtheoretical interpretation is true. That is to say, the underlying similarities between therapeutic modalities in The Handbook of Psychotherapy Integration could be the right interpretation for why psychotherapy works.
I was eager for a chance to ask a researcher I really respect about this. At the Los Angeles County Psychological Association’s annual convention this year, the speaker was Scott D Miller. As one of the authors of The Heart and Soul of Change, he is a major player in the search for the answers to, “what makes psychotherapy work?” and “how can we make it work better?” After his talk, I got the chance to sit down and speak with him.
When I asked him whether psychotherapy was a placebo or whether all the styles of psychotherapy are fundamentally the same, he gave me a response I’m still working to digest. He said, “That kind of thinking continues to look at it through the medical model. I’m only interested in what better facilitates the process of healing.” We went back and forth in our discussion regarding whether psychotherapy has “lost its magick,” with him making impassioned appeals for bringing the art back into the science. He believes we’re too locked into “psychotherapy without art.”
Miller argues that we shouldn’t see ourselves in the narrow profession of ‘psychotherapy’ but in the broader profession of ‘healing.’ This makes me recall reading On Being a Therapist during my master’s program where Jeffrey Kottler romantically describes therapy as a progression of shamanism. Surely the pragmatic philosophy of William James must be driving these people... they have an incredible openness to The Varieties of Religious Experience in order to achieve their goals!
But that’s not the kind of person I am.
VI
I imagine there may be different epistemic personalities. There are people who want everything to be exacting and there are people who can go with the flow and accept ambiguity. Alan Watts has a talk where he refers to this, dividing people as either "prickles" or "goo":
I imagine these personalities leave us with predilections for different cultural projects like science or mysticism, analytic philosophy or continental philosophy.
I’m all prickles. I identify with debunkers like James Randi or Carl Sagan... something about them clicks with my own inner frustrations and anxieties. I am frustrated with the claims people make based on insufficient evidence because of the potential to mislead or harm others. I am anxious about being misled or deceived myself.
And yet there is something to be said for the pragmatists in philosophy for their attempts to resolve the space between prickles and goo. The pragmatist appeal to a coherentist worldview avoids the problems of skepticism we run into when we undertake the prickly Aristotelian project of deriving a foundation from first principles. I have spent a bit of time each week this year trying to better understand the pragmatic underpinnings of the philosopher of science, Willard Van Orman Quine. Quine is quite prickly, describing philosophy as continuous with science and the exploration of science as occurring from within itself with its own tools. And yet he describes science as naught more than another human project, which feels like a gooey way to describe it.
Looking out on the field of psychotherapy from within the philosophy of science I see a problem with our present Research Programme of Evidence Based Practices. Evidence Based Practices rely on conceptualizing psychotherapy with the medical model, where we try to determine which specific ingredients the client’s problem calls for. The research and writing of clinicians like Miller and Wampold directly contradict the utility of specific ingredients, a core part of that model. They show the pragmatic utility of the contextual model in research such as this recent piece by Chow which demonstrates that we can achieve better outcomes when we focus on changing ourselves as clinicians to fit the context in which healing occurs for the client.
This is the stuff scientific revolutions are made of. With such a profound shift in thinking, I still struggle to fit it into my worldview. But I know that as a prickly person, I’m committed to where the evidence leads me. And that as long as I am a clinician, I’m committed to being helpful.