Psychedelic Assisted Therapy and Ketamine Assisted Psychotherapy
When I was a new therapist the biggest questions on my mind were, “how do I ensure I’m helping?” and, “how does therapy work?” I spent a lot of time with textbooks such as The Heart and Soul of Change, and The Great Psychotherapy Debate (which I wrote about in a blog here). This exploration eventually led me to seminars and trainings with Scott D Miller, one of the preeminent experts on Outcomes in Psychotherapy. Since then I have been measuring outcomes in my private practice and routinely collecting feedback in my work using MyOutcomes software in a process known as Feedback Informed Treatment.
After addressing those questions, I’m still asking “how do I better help people?” Scott D Miller and others such as Daryl Chow answer that by telling us to engage in Deliberate Practice - which I think is a pretty good answer! But I think there is also another program in therapy where we are developing practices that dramatically improve the standard of care in therapy: Psychedelic Assisted Therapy, which includes treatments like Psilocybin Assisted Therapy and Ketamine Assisted Psychotherapy (KAP).
I first heard about Psychedelic Assisted Therapy in the early 2000s when I read exciting posts on the internet describing the work coming out from Johns Hopkins University looking at how Psilocybin (magic mushrooms) affected people. They were reporting on research about the positive effects of mystical experiences occasioned by the administration of high doses of Psilocybin, but later they were researching its mental health benefits such as how “Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer.” In addition to universities researching Psilocybin Assisted Therapy, nonprofits like MAPS have been researching Psychedelic Assisted Therapy with a non-classical psychedelic, MDMA (also known as “Ecstasy”). This graphic showing their outcomes for treating PTSD illustrates why I’m so excited about how this sort of seachange could help us improve outcomes:
Right now, only universities and organizations that go through an arduous process of getting approval from the Drug Enforcement Agency can practice with and do research on these substances. That’s because Psilocybin and MDMA, along with most other psychedelics being studied for their therapeutic effects including LSD, 5-MeO-DMT, and Mescaline are considered “Schedule I Substances” by the Drug Enforcement Agency. This means they are federally illegal and considered by the DEA to have, “no currently accepted medical use and a high potential for abuse.”
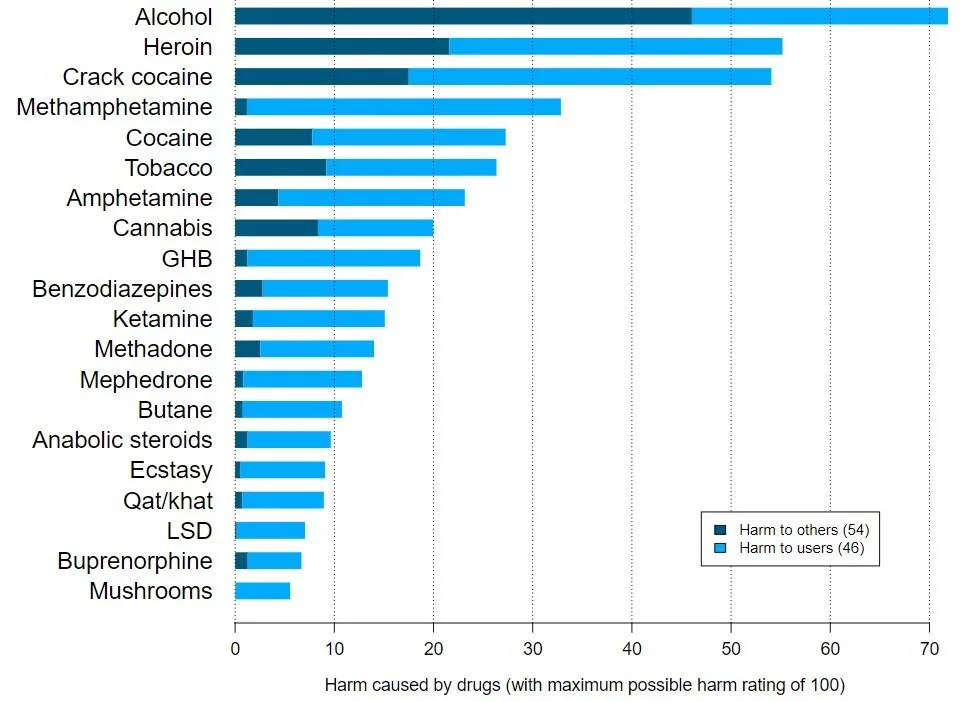
The prohibition on psychedelics is a long story of the culture wars of the 1960s and 70s that continues in an ongoing War on Drugs. Suffice to say, many researchers (and much of the general public) consider the DEA to be flat-out wrong about the medical uses and potential of abuse for psychedelic compounds. They publish papers with graphs like these showing the relative harms of various drugs:
It is notable that LSD, Mushrooms, MDMA are so low on this list, as is ketamine, which is employed in Ketamine Assisted Psychotherapy. This is especially notable compared to the socially acceptable Alcohol, which tops the list. But don’t take this single example as gospel - read other researchers’ takes and look up other discussions on the subject. But I think that review articles like this one, “Assessing the risk-benefit profile of classical psychedelics: a clinical review of second-wave psychedelic research” tell a very tempered story:
“Published studies since 1991 largely support the hypothesis that small numbers of treatments with psychedelic-assisted psychotherapy can offer significant and sustained alleviation to symptoms of multiple psychiatric conditions. No serious adverse events attributed to psychedelic therapy have been reported. Existing studies have several limitations, including small sample sizes, inherent difficulty in blinding, relatively limited follow-up, and highly screened treatment populations.
Substantial data have been gathered in the past 30 years suggesting that psychedelics are a potent treatment for a variety of common psychiatric conditions, though the ideal means of employing these substances to minimize adverse events and maximize therapeutic effects remains controversial.”
We’re starting to have solid knowledge that MDMA, Psilocybin, and other psychedelics help facilitate amazing changes for people who are truly suffering. It’s a shame that these substances remain illegal in the DEA’s list of Schedule I substances. Fortunately, the public is more aware of their potential benefit after the release of bestsellers like Michael Pollan’s How to Change Your Mind, What the New Science of Psychedelics Teaches Us About Consciousness, Dying, Addiction, Depression, and Transcendence.
Psychedelic Assisted Therapy operates a bit differently than either traditional therapy or psychiatry for mental health issues. It involves a series of therapy sessions called preparation, dosing, and integration sessions. Preparation sessions involve education about the effects of the substance to be used, the setting of expectations including intentions for the outcome of treatment, and advice on how to manage the psychedelic experience all while building trust and a relationship between the therapist and client. Dosing sessions are longer than standard therapy sessions and involve the therapist sitting in the office with the client while they are on the substance and occasionally directing them during this experience. Integration sessions are more like typical therapy sessions that focus on debriefing and conversation to understand the experience and reinforce changes that occurred during and since the dosing session. Basically, -’assisted therapy’ means there are a lot of therapy sessions to talk about and understand the implications of the drug experience rather than just using the substance.
Since we’re largely unable to practice with Schedule I substances (the notable exception to this is getting admitted into one of MAPS limited and selective programs for MDMA training), many therapists interested in developing the skills to practice Psychedelic Assisted Therapy are utilizing other substances with some psychedelic effects. Notably the DEA places Ketamine in Schedule III, recognizing it as a substance with medical use that can be safely prescribed by doctors and employed in Ketamine Assisted Psychotherapy.
Ketamine is a dissociative anesthetic that is on the WHO list of essential medicines and has been approved for the treatment of depression. Its standing use in medicine is as an anesthetic, but there’s a recent body of research showing that infusions of ketamine can be helpful for those with treatment-resistant depression (defined as depression that persists despite attempts with at least two different prescribed drugs). Ketamine Assisted Psychotherapy can create nonordinary states of consciousness somewhat like psychedelics do in Psilocybin Assisted Therapy, creating a unique opening to explore the mind, visual and audio hallucinations, dream-like states, and an enhanced sense of connection.
The non-ordinary state of consciousness occasioned by Ketamine administration has led to many therapists beginning to practice Ketamine Assisted Psychotherapy. While this is an interesting experiment, Ketamine is not nearly the same as the classical psychedelics (LSD, Psilocybin, DMT), which interact with the serotonin system. While the action of Ketamine is not completely understood it doesn’t act on the serotonin system, it seems to primarily work on the glutamate system (see LorienPsych’s page on Ketamine).
Ketamine Assisted Psychotherapy is different from the simple administration of a Ketamine infusion. It’s formatted more like how Psychedelic Assisted Therapy works with multiple therapy sessions for preparation, dosing, and integration.
I’ve asked around for research on Ketamine Assisted Psychotherapy, but it seems the evidence is limited as this, Ketamine Assisted Psychotherapy (KAP): Patient Demographics, Clinical Data and Outcomes in Three Large Practices Administering Ketamine with Psychotherapy, is the best article I was given on the subject. I’m looking forward to well controlled future research comparing the outcomes of Ketamine Assisted Psychotherapy to ketamine infusions alone, therapy alone, and ketamine infusions coupled with therapy that does not focus on integrating the ketamine experience. I believe that Ketamine Assisted Psychotherapy will outperform the other groups but I like to refrain from holding strong beliefs until I have strong evidence.
I’m interested in this area because I think it’s the most promising research programme for significantly improving the ability of therapy to help people get where they want to go. I’m interested in the legal and ethical application of utilizing medicines accompanied by therapy to facilitate positive change for those who are suffering and for the betterment of well people. I’ve begun taking courses on Ketamine Assisted Psychotherapy and Psilocybin Assisted Therapy and I’m eager to meet the people actively working in this area.
New Developments in the Approvals of Psychedelic-Assisted Therapy for Veterans with PTSD
We will likely be seeing further developments into the study of psychedelics for conditions such as post-traumatic stress disorder, particularly in the treatment for veterans living with this condition. I am closely following the developments in the Biden administration on this issue, wherein there is an apparent approval by the FDA of MDMA and psilocybin for treating PTSD on the horizon. This would start with “research and pilot programs within the U.S. Department of Veteran Affairs.” Read more about the start of this legislative action here.